How to Manage Treatment-Resistant Bipolar Depression?
Treatment-resistant bipolar depression presents a significant challenge for patients and healthcare providers alike. At Diligence Integrated Care, we understand the complexities of this condition and its profound impact on individuals’ lives.
Our team is committed to exploring advanced strategies and personalized approaches to help those struggling with treatment-resistant bipolar depression. In this post, we’ll delve into the latest research, innovative treatments, and comprehensive management techniques that offer hope for improved outcomes.
What Is Treatment-Resistant Bipolar Depression?
Treatment-resistant bipolar depression presents a complex challenge for individuals with bipolar disorder. This condition affects a significant portion of patients and requires advanced management strategies.
Defining Treatment Resistance
Treatment-resistant bipolar depression occurs when a person with bipolar disorder doesn’t respond to treatment interventions. Over one-third of patients do not respond to treatment, which is commonly known as treatment-resistant bipolar depression. The persistence of depressive symptoms can devastate every aspect of a person’s life.
Dr. Bolanle Oluwadara, MD, observes that patients with treatment-resistant bipolar depression often experience more frequent and longer-lasting depressive episodes. These episodes feature severe mood disturbances, cognitive impairments, and functional disabilities that significantly reduce quality of life.
Prevalence and Impact
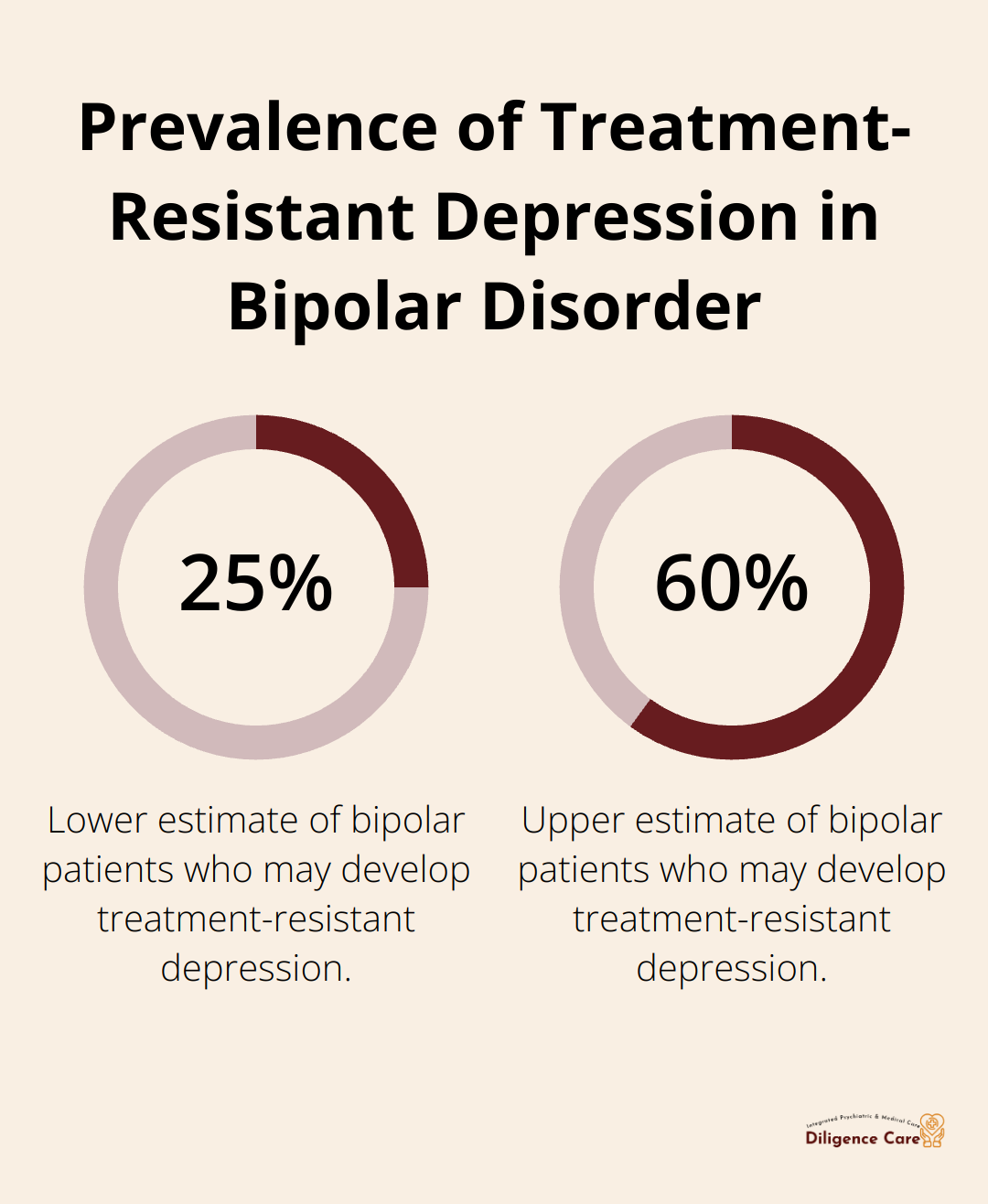
Studies indicate that approximately 25-60% of individuals with bipolar disorder may develop treatment-resistant depression. This high prevalence highlights the urgent need for advanced treatment strategies.
The impact on patients’ lives proves profound. Many struggle to maintain employment, relationships, and daily responsibilities. The risk of suicide also increases significantly in this population. A study found that the likelihood of dying by suicide in bipolar disorder was 8.66 times higher compared to the general population.
Factors Contributing to Treatment Resistance
Several factors can contribute to treatment resistance in bipolar depression. Bernadette Akpengbe, PMHNP-BC, FNP-BC, emphasizes the importance of identifying these factors for effective treatment planning:
Misdiagnosis and Comorbidities
Misdiagnosis occurs frequently. Bipolar depression can be mistaken for unipolar depression, leading to inappropriate treatment. Additionally, comorbid conditions (such as anxiety disorders or substance abuse) can complicate treatment response.
Medication-Related Factors
Poor medication adherence, inadequate dosing, or insufficient time for medications to take effect can all contribute to apparent treatment resistance. Sometimes, the chosen medications may not prove most effective for a particular individual’s genetic makeup or symptom profile.
Biological and Environmental Factors
Certain biological factors, such as alterations in brain structure or function, can influence treatment response. Environmental stressors, poor sleep habits, and lack of social support can also hinder recovery.
Tony Akpengbe, DNP, works diligently to ensure accurate diagnosis, appropriate medication management, and holistic care that addresses both biological and environmental influences on bipolar depression.
Understanding the complexities of treatment-resistant bipolar depression forms the foundation for developing effective management strategies. The next section will explore comprehensive diagnostic approaches that pave the way for successful treatment plans.
Unraveling the Diagnostic Puzzle
Beyond Surface Symptoms
Dr. Chijioke Iwuchukwu, MD, stresses the importance of looking beyond surface-level symptoms. Many medical conditions can mimic or exacerbate bipolar depression. Thyroid disorders can exacerbate or mimic the symptoms of bipolar disorder. Research indicates that thyroid hormones play a crucial role in mood regulation. We conduct thorough medical evaluations, including blood tests and imaging studies when necessary, to rule out underlying health issues.
Uncovering Hidden Comorbidities
Comorbid psychiatric disorders often complicate bipolar depression treatment. Anxiety disorders, substance use disorders, and personality disorders frequently co-occur with bipolar disorder. These conditions can mask bipolar symptoms or interfere with treatment efficacy. Our team uses structured diagnostic interviews and validated assessment tools to identify and address these comorbidities. For example, the RMS-C is a valid, simple self-administered screening tool to help identify BD-I or BD-II in persons experiencing a depressive episode.
Medication Detective Work
Treatment resistance sometimes stems from medication-related issues rather than the condition itself. We meticulously review patients’ medication histories, looking for:

Eric Efuetngu, DNP, FNP-C, APRN, notes that up to 60% of bipolar patients struggle with medication adherence at some point. We work closely with patients to address barriers to adherence and optimize their medication regimens.
Lifestyle Factors Under the Microscope
Lifestyle factors play a significant role in treatment outcomes. We assess sleep patterns, diet, exercise habits, and stress levels. Mavis Efuetngu, PMHNP-BC, APRN, points out that disrupted circadian rhythms can significantly impact mood stability in bipolar disorder (often leading to more frequent episodes). We help patients implement lifestyle modifications that support their treatment goals.
Genetic and Biomarker Insights
Emerging research suggests that genetic factors and biomarkers may influence treatment response in bipolar depression. While not yet standard practice, we stay informed about these developments and may recommend genetic testing in certain cases to guide medication selection.
Our comprehensive diagnostic approach leaves no stone unturned. We address medical comorbidities, uncover hidden psychiatric conditions, optimize medication regimens, and consider lifestyle factors. This thorough evaluation process sets the stage for the advanced treatment approaches we’ll explore next. Let’s examine how these strategies can make a real difference in managing treatment-resistant bipolar depression.
Innovative Approaches for Stubborn Bipolar Depression
Treatment-resistant bipolar depression requires a multifaceted approach. We employ cutting-edge strategies to help patients find relief and stability.
Tailored Medication Combinations
Dr. Bolanle Oluwadara, MD, emphasizes the importance of personalized medication regimens. We often combine mood stabilizers (like lithium or valproic acid) with atypical antipsychotics (such as quetiapine or lurasidone). This combination targets both depressive symptoms and mood instability.
A 2022 study in the Journal of Affective Disorders found that combining lithium with an antipsychotic led to a 65% response rate in treatment-resistant cases. We monitor patients closely, adjust dosages and combinations to maximize benefits while minimizing side effects.
Psychotherapy as a Powerful Adjunct
Medication alone often isn’t enough. Bernadette Akpengbe, PMHNP-BC, FNP-BC, integrates evidence-based psychotherapies into treatment plans. Cognitive Behavioral Therapy (CBT) helps patients identify and change negative thought patterns. Interpersonal and Social Rhythm Therapy (IPSRT) focuses on stabilizing daily routines and improving relationships.
A meta-analysis published in JAMA Psychiatry showed that adding psychotherapy to medication reduced relapse rates by 30% in bipolar disorder. We offer both individual and group therapy options, tailoring the approach to each patient’s needs and preferences.
Breakthrough Treatments: Ketamine and TMS
For patients who don’t respond to traditional therapies, we explore innovative options. Repeated esketamine infusions may help reduce depressive symptoms in hospitalized patients with moderate to severe bipolar depression within two weeks.
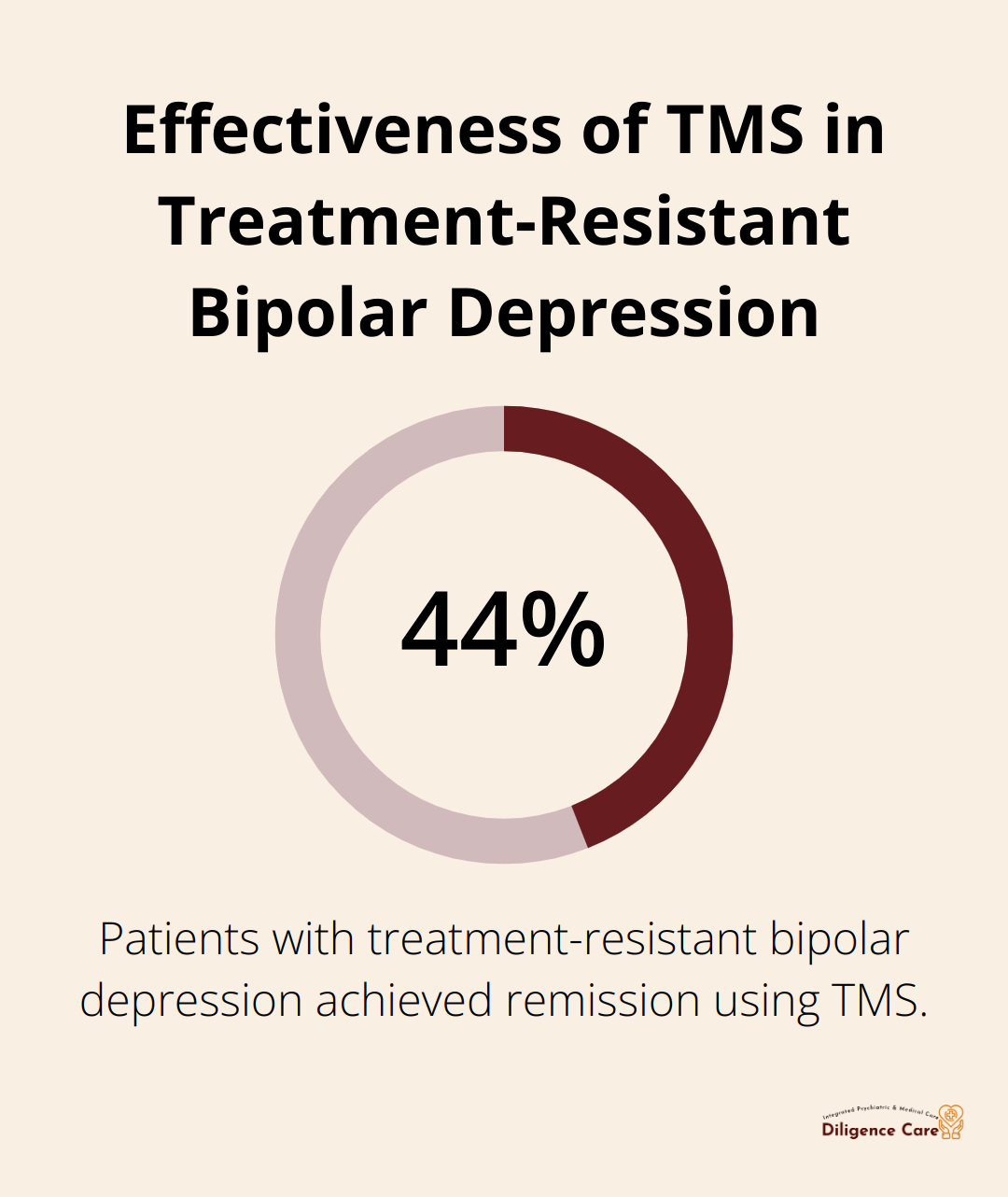
Transcranial Magnetic Stimulation (TMS) offers another non-invasive option. Dr. Chijioke Iwuchukwu, MD, notes that TMS can be particularly effective for patients who can’t tolerate medication side effects. A recent trial found that 44% of treatment-resistant bipolar depression patients achieved remission with TMS.
These treatments show promise but require careful consideration and close monitoring. We thoroughly evaluate each patient’s suitability for these advanced therapies.
Holistic Lifestyle Interventions
Medication and therapy form the core of treatment, but lifestyle factors play a significant role. Mavis Efuetngu, PMHNP-BC, APRN, works with patients to implement evidence-based lifestyle changes:
- Sleep optimization: Consistent sleep-wake cycles are vital for mood stability. We use sleep hygiene techniques and sometimes prescribe sleep aids to regulate circadian rhythms.
- Exercise regimens: Regular physical activity boosts mood and energy levels. A study in the Journal of Psychiatric Research found that aerobic exercise three times a week reduced depressive symptoms by 40% in bipolar patients.
- Nutrition counseling: We guide patients towards anti-inflammatory diets rich in omega-3 fatty acids, which have been linked to improved mood stability.
- Stress management: Techniques like mindfulness meditation and progressive muscle relaxation help patients cope with stress (a common trigger for mood episodes).
Our comprehensive approach combines pharmacological innovation, targeted psychotherapy, cutting-edge treatments, and lifestyle modifications. We work closely with each patient, adjust strategies as needed to achieve the best possible outcomes.
Final Thoughts
Treatment-resistant bipolar depression challenges patients and healthcare providers. Diligence Integrated Care offers personalized treatment plans that combine medication, therapy, and lifestyle changes. Our team adjusts strategies to find the most effective approach for each individual, even when progress seems slow.
Research expands our understanding of bipolar disorder and treatment resistance. We integrate promising new approaches into our treatment plans when appropriate. Support extends beyond the clinical setting, and we emphasize the importance of building a strong network of family, friends, and support groups.
Diligence Integrated Care provides comprehensive care for individuals struggling with treatment-resistant bipolar depression. Our integrated approach addresses mental and physical health (ensuring every aspect of a patient’s well-being is considered). With personalized treatment plans and cutting-edge therapies, we help patients work towards stability and improved quality of life.